Psychedelic Therapy for Trauma and Post Traumatic Stress Disorder
Trauma and PTSD are mental health issues that are receiving more attention from the media and clinicians.
And this rise in awareness comes at a good time.
In 2020, 13 million Americans had PTSD. [1]
Individuals can develop post traumatic stress disorder (PTSD) from acute, personal events or from larger-scale, societal happenings, such as war, a pandemic, or an economic recession.
Today, people are seeking healing for their trauma and looking for alternatives as traditional treatments have proven ineffective for many. [2]
Psychedelic drugs are one such alternative. These plant medicines have significant clinical benefits and their therapeutic potential is extremely high.
In this article, we'll explore how psychedelic-assisted therapy for healing trauma and PTSD works and why it might be the most effective treatment ever discovered.
What is Trauma and PTSD?
Quick Note: This section explores defining the terms “trauma” and “PTSD”. If you think you’re adequately familiar with these terms, then feel free to skip ahead to the next section.
Generally speaking, trauma is the felt pain connected to a challenging experience or event.
The most commonly reported traumatic events are:
Witnessing a serious injury or death
The loss of a loved one unexpectedly
Being physically attacked
Experiencing a life-threatening car accident
Personally experiencing a life-threatening illness or injury [3]
After a severely challenging experience (like those listed above), someone might feel that they are suffering emotionally, somatically, spiritually, and so forth.
We call this pain and suffering “trauma”.
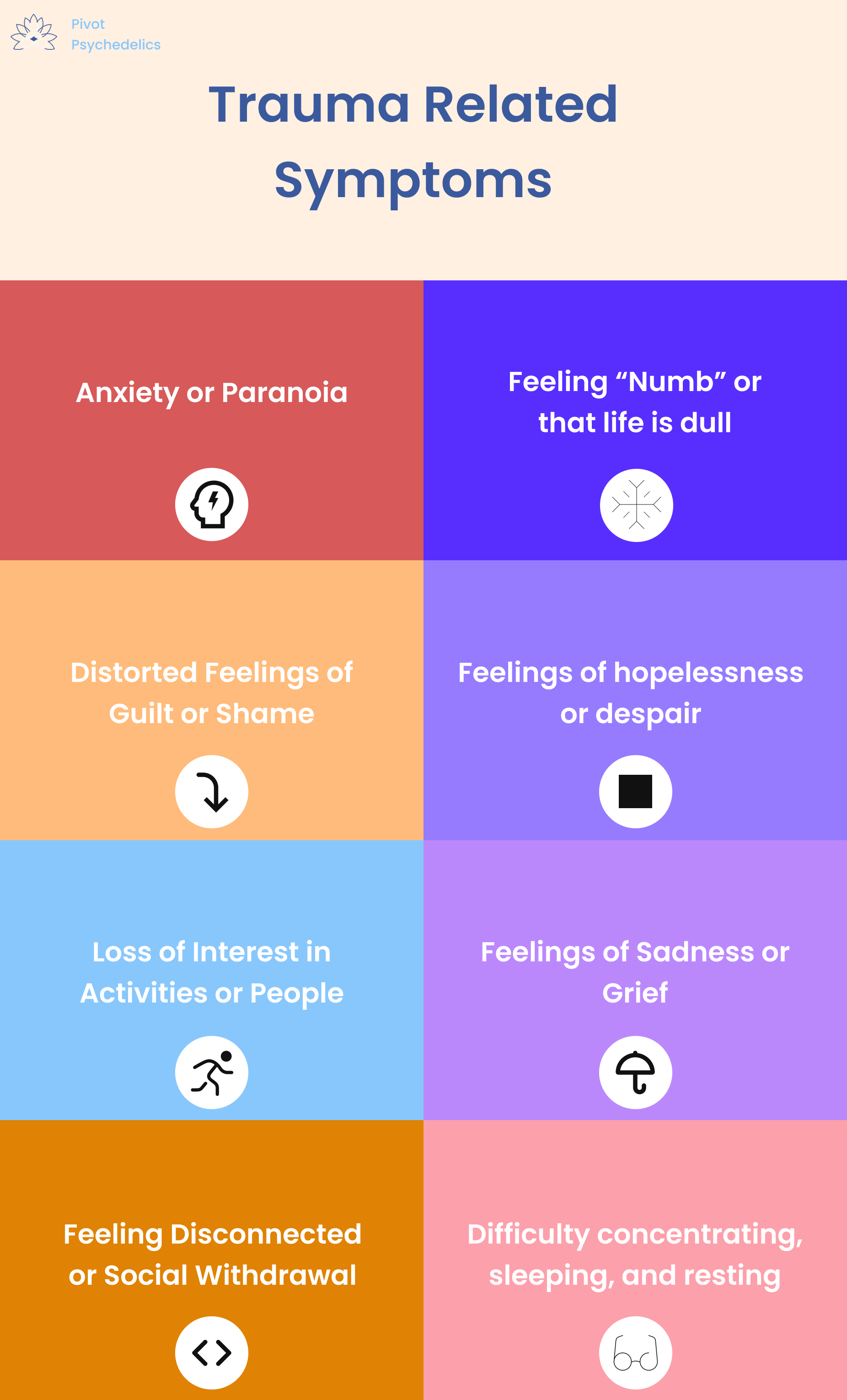
Trauma can show up in ways that are physical, mental, emotional, and behavioral. Here are the common symptoms that can be directly related to trauma:
Avoidance of activities, places, or people that trigger traumatic memories of
Flashbacks of the traumatic event
Intrusive thoughts and images
Distressing dreams related to trauma
Sometimes trauma-related effects take shape in us in less obvious or direct ways.
In these instances, trauma symptoms might include:
Anxiety or paranoia
Distorted feelings of guilt or shame
Loss of interest in activities or people
Feeling disconnected or experiencing social withdrawal
General "numbness" or feeling that life is dull
Feelings of hopelessness or despair
Feelings of sandess or grief
Difficulty concentrating, sleeping, or resting
As you might expect, there's often overlap between trauma and other mental illnesses. Some of the most common issues include anxiety, depression, and alcohol use disorder. [4] [5]
Trauma can come in many forms, including acute experiences and chronic ones. The intensity and severity of either kind can lead one to post traumatic stress disorder or "PTSD" for short.
A medical professional, like a psychiatrist, can diagnose individuals with PTSD.
How Common Is Trauma?
Trauma is extremely common.
In a global survey of 24 countries in six different continents, 70% of respondents reported a traumatic experience in their life. [6]
We used to think trauma was caused only by single, significant adverse events, like being physically attacked or losing a loved one.
With this understanding, only those affected by individual, intense moments, such as sexual assault survivors or veterans, would have trauma.
What we've come to learn is that trauma can be experienced in singular or compounding events, at all stages of the life cycle. Here are some ways emotional trauma can build up over many instances:
In a marriage, one partner feels emotionally attacked by the other
A student at a school gets bullied regularly by peers
An LGTBQ+ individual experiences discrimination in severe and subtle ways
Similarly, there are a variety of risk factors that contribute to the development of PTSD. [7]
Trauma is something that affects us all, directly or indirectly.
There's a whole field of research dedicated to understanding trauma that is passed down in one's ancestral lineage, called "intergenerational trauma". [8]
In summary, there are a variety of types of trauma and degrees of severity, from a comorbid mental health disorder to chronic PTSD.
How PTSD is Treated Today
There are two common ways PTSD is treated in the Western medical model:
Psychotherapy
Pharmaceuticals, like antidepressants
Therapy for Trauma
Psychotherapy, also referred to as "talk therapy" or just "therapy", involves the client meeting with a practitioner like a therapist, social worker, or counselor.
Therapy takes time to establish a trustworthy relationship and explore the elements of trauma that are challenging for the client.
The purpose of therapy for treating trauma is to help clients move towards a place of safety and help people cope with their trauma in healthier ways.
For example, if someone experienced physical and emotional trauma in a natural disaster, they may feel a lack of security and safety in relation to others. A therapist can serve as a trusted professional who demonstrates empathy and compassion to help the client rebuild confidence in others.
Additionally, a client might work with the therapist on reshaping how they think about their trauma.
The main idea here is that how one thinks about a particular instance, memory, or trigger is a learned behavior. And if it's been learned, then it can be unlearned.
Common psychotherapeutic techniques to accomplish this include Cognitive Behavioral Therapy and Cognitive Processing Therapy
Pharmaceuticals for Trauma
The FDA-approved treatment for PTSD is the prescription of antidepressants.
Antidepressants help individuals feel less stress.
Selective serotonin reuptake inhibitors (SSRIs) are one common type of antidepressant.
Serotonin-norepinephrine reuptake inhibitors (SNRIs) are also common.
Most people take these medicines daily and check in with their prescribing psychiatrist to track symptoms and adjust dosage as necessary.
Limitations of PTSD Treatment
There are four major criticisms of these traditional treatment options, two for talk therapy and two for pharmaceuticals
#1 Talk therapy can only do so much.
Some people find that therapy helps them think differently, but not feel differently. Therapy can help someone understand where their trauma comes from and what their triggers are, but for some people it falls short of actually helping them heal.
What's more, many patients with PTSD fail to respond to the therapy or dropout of therapy altogether. [9]
#2 Talk therapy takes a long time.
Working with a therapist requires lots of time and energy to build rapport, dive into one's inner world, and rework thought patterns. This process can take years.
#3 Antidepressants only address symptoms, not the root cause of issues.
If you're feeling overwhelmed by trauma, SSRIs and other antidepressants can be extremely helpful in addressing your symptoms. However, this can be like a temporary fix rather than a long-term solution.
Similar to talk therapy, the efficacy of this treatment isn't guaranteed. An estimated 40-60% of PTSD patients do not experience benefit from these medicines. [10]
#4 Antidepressants are difficult to stop taking.
Antidepressants must be taken daily and consistently to have an effect. Once an individual starts taking them, it's likely that they'll continue taking them because tapering these meds can have unpleasant side effects.
With these limitations in mind, clients and their clinicians are turning towards alternatives. One promising option: psychedelic drugs + psychedelic assisted therapy.
How Psychedelics Treat PTSD
Psychedelic medicine like magic mushrooms, LSD, and MDMA are being studied to treat a variety of mental health disorders, including PTSD.
So far, the results are extremely promising.
One reason why researchers believe psychedelics can treat PTSD, is that psychedelics promote neural growth.
In our brains, we have millions of neurons that "talk" to each other. Psychedelics can actually stimulate the creation of new neurons in a process called neurogenesis.
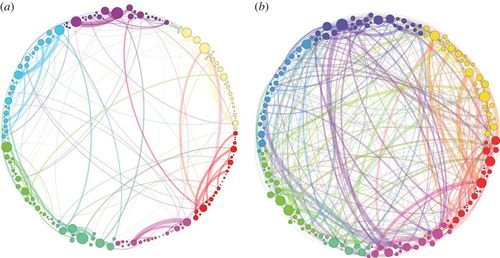
A helpful illustration for this comes a 2014 research paper on psychedelics and brain functional networks: [11]
This image, made popular in Michael Pollan's book How To Change Your Mind, demonstrates the increased brain wiring involved in a psychedelic experience (right) compared to a brain who received a placebo (left).
The greater communication between different parts of the brain in a psychedelic experience could be what makes the trip so therapeutically beneficial. Here's how these changes could be helpful for PTSD:
Change In Thought Patterns - New, healthier thinking occurs, breaking negative thought loops and intrusive thoughts
Easier Processing of Trauma - Otherwise difficult mental health content can be processed in a safe environment with professional support
Emotional Release - This processing can lead to catharsis and relief, especially for suppressed feelings related to trauma
Fear Extinction - Challenging triggers can lose their hold on the mind as people open up to new possibilities. [12]
These experiences, while not guaranteed for everyone, are commonly reported in clinical trials and intentional use.
MDMA and other psychedelic drugs may be key tools that become our most effective treatments for trauma.
Psychedelic therapies have vast healing potential for trauma and they may help us heal in other significant ways.
Can Individuals Heal PTSD + Anxiety or Depression at the Same Time?
With trauma, there's often overlap with other mental health issues like generalized anxiety, major depressive disorder (MDD), and substance abuse.
We at Pivot often hear from clients the question
"Can psychedelics help with multiple things?"
The answer is most often yes.
Psychedelics act as "non-specific amplifiers", so they take whatever we have in our conscious and subconscious minds and make them seem more intense, perceptually or affectively.
A psychedelic experience can bring up a large amount of psychological material. Here's an example of what one Pivot client reported during their experience:
Childhood memories related to their trauma
Visions of birds in flight and felt sense that they were soaring with them
Anxiety about dating and seeing this as somewhat silly
Distorted replay of a TV show they watched the night prior
A vision of masks falling from peoples' faces to reveal their authentic selves
As you can see, in just one experience there were vastly different elements of their consciousness that came up. Ultimately, some of it related to mental health issues directly, including trauma, and some of it was less apparent.
However, this client moved through the Integration Process (LINK) and came to understand themes of their experience that connected in unexpected ways. Here were some connections they drew:
Childhood trauma --> Need for approval
Dating anxiety --> Also a desire for approval
Need for approval --> Blocker to their happiness
Moving past approval --> Masks falling away / authenticity
Authenticity --> Flying high, a metaphor for living their best life
Making connections like these can help us immensely in healing.
Often, individuals go through a psychedelic experience and become more aware of their inner world.
As it relates to trauma, our "other" emotional health, physical health, and wellness material is often interwoven.
The positive effects of psychedelics can be immensely helpful in rethinking traumatic memories, supporting the brain's ability to adapt, and increasing positive psychoactive effects.
Clinical Trials and MAPS
Despite heaps of anecdotal experience and years of research in the 20th and 21st centuries, psychedelic drugs are not yet approved medicines for treating PTSD.
Rigorous psychedelic research has been conducted on MDMA assisted therapy for PTSD through the non-profit the Multidisciplinary Association for Psychedelic Studies (MAPS).
One brief note is that "MDMA" stands for 3,4-methylenedioxymethamphetamine. Other common names for this psychedelic drug are "ecstasy" and "molly".
In 21st century pop culture, MDMA's been considered a "party drug", but we're seeing medical institutions and governing bodies rethinking this limited framework.
The Food and Drug Administration (FDA) approved the fast track of MDMA drug development to treat patients with PTSD in 2016. This designation is known as "breakthrough therapy". [13]
Groundbreaking results came from MAPS studies in 2019. Six phase 2 studies conducted controlled trials to evaluate the efficacy of MDMA assisted therapy for treating PTSD in 103 participants. Results showed that over half of participants who received MDMA no longer met the criteria for PTSD - in other words, they were cured. [14]
Clinical trials then expanded to phase 3.
In a 2021 MAPS study, researchers found that MDMA-assisted therapy was highly effective at treating severe PTSD compared to therapy with the placebo group. Additionally, the MDMA did not induce likelihood of abuse potential or suicidality. [15]
It's quite possible that the FDA will approve a protocol for MDMA therapy to treat PTSD soon. In these cases, people who have access to health insurance could gain access to these medicines through a doctor's prescription.
For now, people are seeking healing for their PTSD and using psychedelics with psychedelic guides or professionals.
Psychedelic Treatment Available Right Now
If you're looking for a psychedelic experience to treat PTSD or other mental health issues, there are a few options available:
Travel Abroad - While most psychedelic drugs remain illegal in the United States, there are several countries where these medicines are permissible. Groups such as Heroic Hearts foundation and VETS provide opportunities for veterans. One common place for people to pursue psilocybin treatment is Jamaica.
Ketamine for Anxiety and Depression - Ketamine is an anesthetic which has psychedelic properties, so it's largely considered a psychedelic drug. It's approved for label use to treat anxiety and depression. Most major U.S. cities have ketamine clinics, but many clinics do not provide therapeutic support directly.
Guided Psychedelic Experience - People all over the U.S. are using psychedelics intentionally to heal. Typically, they're pursuing this work with a psychedelic therapist or a guide who can support them on their journey. Legality here varies by state and jurisdiction.
Many clients have success when they consider the option that best fits their goals. It's also critical that you're familiar with safety and legal frameworks when doing this work.
Psychedelic treatments and psychedelic psychotherapy are gaining popularity, but it can be hard to know where to start.
An expert in psychedelics can help you in your discernment process and ensure that you are informed on your options.
If you're looking for a guided psychedelic experience, you can request a free consultation with Pivot Psychedelics. We provide guided psychedelic experiences, including therapeutic support with ketamine.
Disclaimer: While the body of research around psychedelic treatment for trauma and PTSD is growing, many substances remain federally illegal in the United States. None of the information presented in this article is an endorsement of illicit drug use. No content, including this blog past, from Pivot Psychedelics is medical advice nor an adequate substitute for it. Please consult with a medical professional if you are experiencing issues related to trauma.
Sources:
How Common Is PTSD in Adults?. (n.d.) U.S. Department of Veteran Affairs. www.ptsd.va.gov/understand/common/common_adults.asp
Gutner, C. A., Gallagher, M. W., Baker, A. S., Sloan, D. M., & Resick, P. A. (2016). Time course of treatment dropout in cognitive–behavioral therapies for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 8(1), 115–121. doi:10.1037/tra0000062
Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A., Ruscio, A. M., Shahly, V., Stein, D. J., Petukhova, M., Hill, E., Alonso, J., Atwoli, L., Bunting, B., Bruffaerts, R., Caldas-de-Almeida, J. M., de Girolamo, G., Florescu, S., Gureje, O., Huang, Y., Lepine, J. P., … Koenen, K. C. (2016). The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychological medicine, 46(2), 327–343. doi:10.1017/S0033291715001981
Hegel, M. T., Unützer, J., Tang, L., Areán, P. A., Katon, W., Noël, P. H., Williams, J. W., Jr, & Lin, E. H. (2005). Impact of comorbid panic and posttraumatic stress disorder on outcomes of collaborative care for late-life depression in primary care. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry, 13(1), 48–58. doi:10.1176/appi.ajgp.13.1.48
Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic Stress Disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi:10.1001/archpsyc.1995.03950240066012
Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A., Ruscio, A. M., Shahly, V., Stein, D. J., Petukhova, M., Hill, E., Alonso, J., Atwoli, L., Bunting, B., Bruffaerts, R., Caldas-de-Almeida, J. M., de Girolamo, G., Florescu, S., Gureje, O., Huang, Y., Lepine, J. P., … Koenen, K. C. (2016). The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychological medicine, 46(2), 327–343. doi:10.1017/S0033291715001981
Yehuda, R., Flory, J.D., Pratchett, L.C. et al. Putative biological mechanisms for the association between early life adversity and the subsequent development of PTSD. Psychopharmacology 212, 405–417 (2010). doi:10.1007/s00213-010-1969-6
Yehuda, R., & Lehrner, A. (2018). Intergenerational transmission of trauma effects: putative role of epigenetic mechanisms. World psychiatry : official journal of the World Psychiatric Association (WPA), 17(3), 243–257. doi:10.1002/wps.20568
Bisson, J. I., Roberts, N. P., Andrew, M., Cooper, R., & Lewis, C. (2013). Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. The Cochrane database of systematic reviews, 2013(12), CD003388. doi:10.1002/14651858.CD003388.pub4
Steenkamp MM, Litz BT, Hoge CW, Marmar CR. Psychotherapy for Military-Related PTSD: A Review of Randomized Clinical Trials. JAMA. 2015;314(5):489–500. doi:10.1001/jama.2015.8370
Petri, G., Expert, P., Turkheimer, F., Carhart-Harris, R., Nutt, D., Hellyer, P. J., & Vaccarino, F. (2014). Homological scaffolds of brain functional networks. Journal of the Royal Society, Interface, 11(101), 20140873. doi:10.1098/rsif.2014.0873
Hake, H. S., Davis, J. K. P., Wood, R. R., Tanner, M. K., Loetz, E. C., Sanchez, A., Ostrovskyy, M., Oleson, E. B., Grigsby, J., Doblin, R., & Greenwood, B. N. (2019). 3,4-methylenedioxymethamphetamine (MDMA) impairs the extinction and reconsolidation of fear memory in rats. Physiology & behavior, 199, 343–350. doi:10.1016/j.physbeh.2018.12.007
Feduccia, A. A., Jerome, L., Yazar-Klosinski, B., Emerson, A., Mithoefer, M. C., & Doblin, R. (2019). Breakthrough for Trauma Treatment: Safety and Efficacy of MDMA-Assisted Psychotherapy Compared to Paroxetine and Sertraline. Frontiers in psychiatry, 10, 650. https://doi.org/10.3389/fpsyt.2019.00650
Mithoefer, M.C., Feduccia, A.A., Jerome, L. et al. MDMA-assisted psychotherapy for treatment of PTSD: study design and rationale for phase 3 trials based on pooled analysis of six phase 2 randomized controlled trials. Psychopharmacology 236, 2735–2745 (2019). doi:10.1007/s00213-019-05249-5
Mitchell, J.M., Bogenschutz, M., Lilienstein, A. et al. MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study. Nat Med 27, 1025–1033 (2021). doi:10.1038/s41591-021-01336-3