Psychedelic Therapy for Depression
Psychedelics are mind altering medicines that have been used by humans for thousands of years to initiate or commemorate change.
In popular media today, psychedelic drugs are often discussed as therapeutic tools to help change someone's mindset, including bring benefit to their mental health.
Clinical researchers in behavioral sciences are studying the efficacy of psilocybin treatment and other psychedelics for treating depression, anxiety, trauma, and more.
What's amazing about these medicines and the studies around them is the treatment isn't just concerned with managing symptoms, it's about curing symptoms.
Many current forms of treatment, such as antidepressants, are geared to help people with their symptoms, e.g., stabilize their mood.
Psychedelic treatment on the other-hand is set up to help people address the root causes of their underlying issues. Psychedelic therapy is showing incredible promise for treating depression. [1]
In this article, we'll cover more on psychedelic medicine research and mental health. We also talk about intentional use of psychedelics, such as magic mushrooms, outside of clinical trials.
Finally, we'll give some parting words on how you can maximize the therapeutic benefits of these medicines to help with depression.
What is Depression?
We can use words like sadness and grief to describe depression.
When we think of depression, we could see it as something that we all experience from time to time or as something people are clinically diagnosed with.
Everyone can experience sadness of some kind, though some people may be a bit more predisposed to severe forms of it.
We'll cover what depression can look like for someone who encounters general Life Challenges.
Then, we'll go over what we mean by clinical depression with discussion around various types of depression including Treatment Resistant Depression, Major Depression, and Other Depressive Disorders.
Life Challenges
Everyone can feel depressed from time to time.
These are very real events, circumstances, or issues of the human experience that can lead someone to experience depressive symptoms.
Some examples include rejection, loss, lack of meaning, or feeling lost.
Most people will experience some of these life challenges during their time on earth.
Do these people have 'depression? While they may not in a clinical sense, it's certainly possible that they feel depressed.
When people go through challenging times, it's not uncommon for them to display some depressive symptoms, such as lack of interest in people or things.
Depending on the severity of the situation and the person coping with it, major depressive disorder may or may not develop.
It's our perspective that depression is both a combination of genetic predisposition (nature) and environmental conditions (nurture).
For this reason, we will often work with "healthy normals", or people without clinical diagnoses, to help them work through life challenges.
In this process, we accept our sadness or grief, commit to processing it, and engage in healthy coping behaviors (e.g., meditation, social connection, psychedelic integration) then we set ourselves up for both adequately honoring our lived experience and building a mindset that can find peace.
Treatment Resistant Depression, Major Depression, and Other Depressive Disorders
For some people, depression is something they've had for a long time.
In the Western medical world, these individuals might be given a clinical diagnosis. They're likely prescribed medications, like antidepressants, and advised to pursue psychotherapy.
Depression in this clinical sense can be defined as a mood disorder that comes with persistent feelings of sadness that negatively affect how you think, act, sleep, etc.
There are several types of categories used to describe this mental health condition. [2]
Here are a few:
Major Depressive Disorder (MDD) - depression that leaves one feeling sad almost all of the time for a minimum of two weeks and comes with detriments to health and wellness, such as a loss of sleep.
Treatment Resistant Depression (TRD) - a subset of MDD, where depression does not get better after traditional treatment options, such as talk therapy and pharmaceuticals. [3]
Persistent Depressive Disorder (PDD) - mild or moderate depression that lasts a minimum of two years, though symptoms are less severe than MDD.
Seasonal Affective Disorder - depression that's linked to the changing of seasons, usually rising during fall and winter.
Prenatal depression and postpartum depression - depression that happens during (i.e. prenatal) or after (i.e. postpartum) pregnancy.
When individuals have tried several treatment options, yet their symptoms persist then a diagnosis of treatment resistant depression may be given.
As the name suggests, conventional treatment options have not worked or at least have not worked very well in these cases.
This diagnosis can bring about feelings of hopelessness and helplessness. Individuals facing major depression might feel like they're on an island.
Conventional treatment seems to have hit a limit to its healing potential, and researchers have asked the question:
What else could be effective for
treating major depressive disorder?
One of the most promising treatments is psychedelic-assisted therapy.
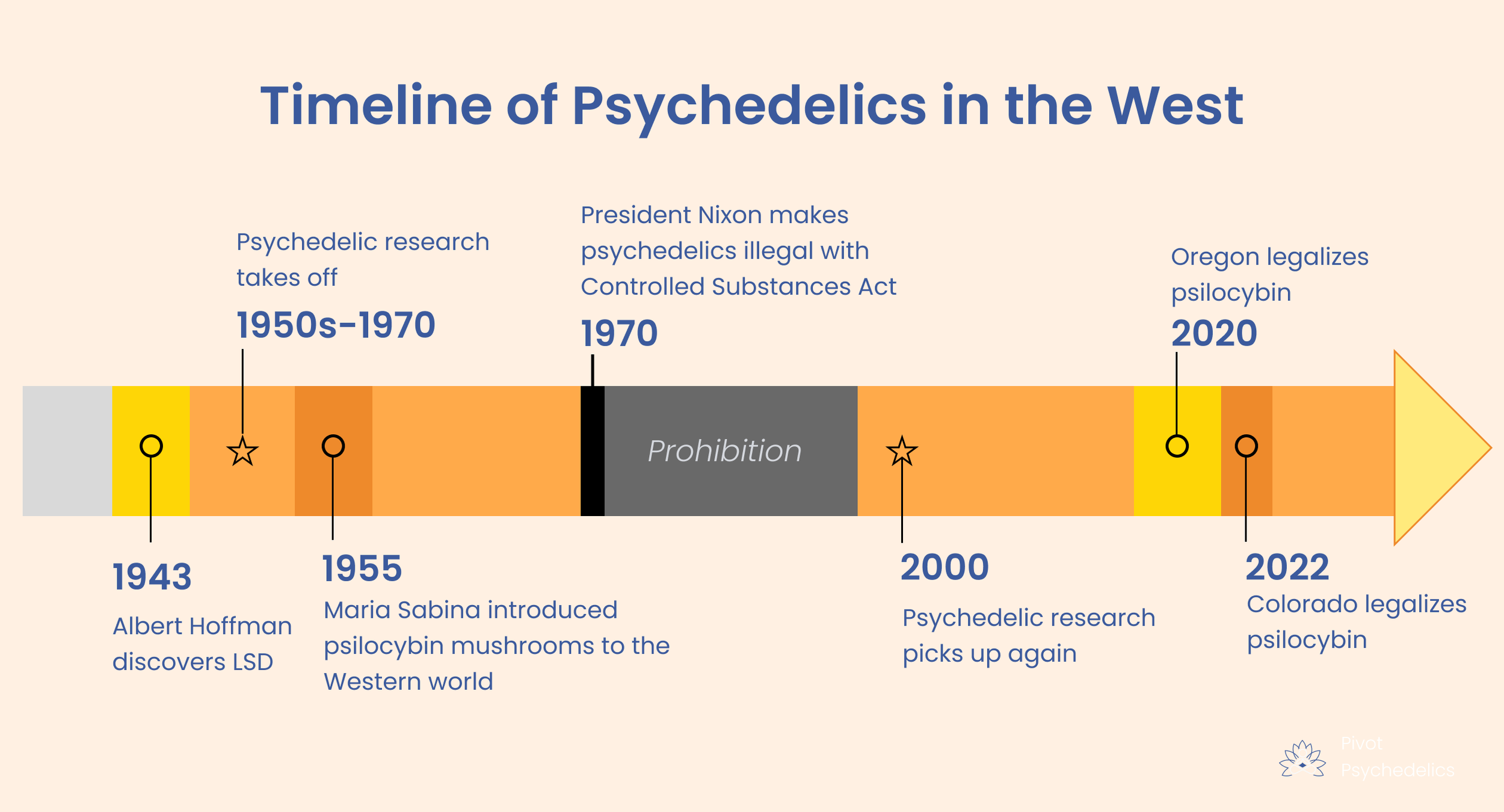
The History of Psychedelic Drugs for Depression
Psychedelic drugs were studied for several decades in the 20th century. They were found extremely effective for treating depression, facilitating mystical experiences, and helping people quit drinking and substance use. [4]
It seemed like we were on the path towards a new medical paradigm that would open up the most effective healing methods ever studied.
But it was all shut down by former president Nixon, who made base-less claims against these medicines. Former Nixon administrator, domestic policy chief John Ehrlichman, confirmed that this decision was solely political as an attempt to silence progressive ideology that promoted policy to help middle-class Americans, Black people, and the majority of American citizens more broadly. [5]
Did psychedelic-assisted therapy vanish?
Thankfully, no. While these overwhelming safe, therapeutically beneficial medicines were made illegal, several factions of clinicians and therapists continued to work with them in the underground.
They continued to bring psychedelics to their clients to treat anxiety, substance use, and depression.
Around the turn of the 21st century, researchers at Johns Hopkins University and others at prominent institutions were granted government permission to study psychedelics once more.
After decades of stalled progress, psychedelic science was back up and running. And over the last two decades, researchers have seen amazing results for psychedelic-assisted therapy to help treat depression, end-of-life anxiety, substance use, and PTSD, to name a few. [6]
For depression in particular, the research results are astounding.
In the largest-ever psilocybin treatment study for depression, researchers found that 37% of participants had their depressive symptoms fall by at least 50%. What's more, 29% of participants were in full remission after 3 weeks - meaning they had no more depression. [7]
Psychedelic use outside of medical settings may also carry great benefits.
In two studies, researchers found that citizen psychedelic use (i.e. not in a clinical trial or medical setting) indicated significant decreases in experiential avoidance, depression severity, and suicidal ideation. [8]
In observational studies, psychedelic experiences led to elevated well-being scores, such as positive affect, self-esteem, resilience, and mindfulness, a full 2 years after an experience. [9]
Psychedelics vs Selective Serotonin Reuptake Inhibitors (SSRIs)
Psychedelics are gaining traction in the medical community because they are almost twice as effective as traditional treatment for depression.
When clinicians speak about depression, treatment with SSRIs and antidepressants help ensure symptoms are "managed". These medicines can help people reduce their feelings of depression in the short term.
Psychedelics on the other hand help people with the underlying causes or issues that lead to depression. Through psychedelic-assisted therapy, people can journey deep into their psyche and work through the source of their mental pain.
For this reason, clinicians and researchers speak about psychedelics and use the term "cure".
Not surprisingly, most people are more interested in curing their depression than managing it. Here’s a useful graphic to understand the two different approaches:
Research on Psychedelics, Antidepressants, and Therapy
Psychedelic treatment is suggested to be extremely effective after just one session with guidance before and after. [10]
SSRIs on the other hand can take several weeks before effects are felt. [11]
Now, it's important to note that SSRIs can be an effective treatment for depression. [12]
Even if the positive effects don't happen immediately, these medicines can help patients maintain stability.
Another method of healing worth mentioning is psychotherapy. An intervention such as cognitive behavioral therapy, can support patients by helping them work through psychological patterns and disrupt unhelpful thinking mechanisms. [13]
So are psychedelic treatments more effective?
We need more research on these drugs and their impact on psychiatry, but the evidence so far favors psychedelics.
Studies conducted by Johns Hopkins Medical center showed that psilocybin treatment with psychotherapy helped relieve major depressive disorder (MDD) symptoms for at least a year in some patients. [14]
Ultimately, each person's response to medicine is unique, and it's essential that people work with medical professionals and doctors to ensure safety when making a decision about these medicines.
How Psychedelic Assisted Therapy for Depression Works
Okay, it might sound great that psychedelic therapy like psilocybin treatment helps with depression.
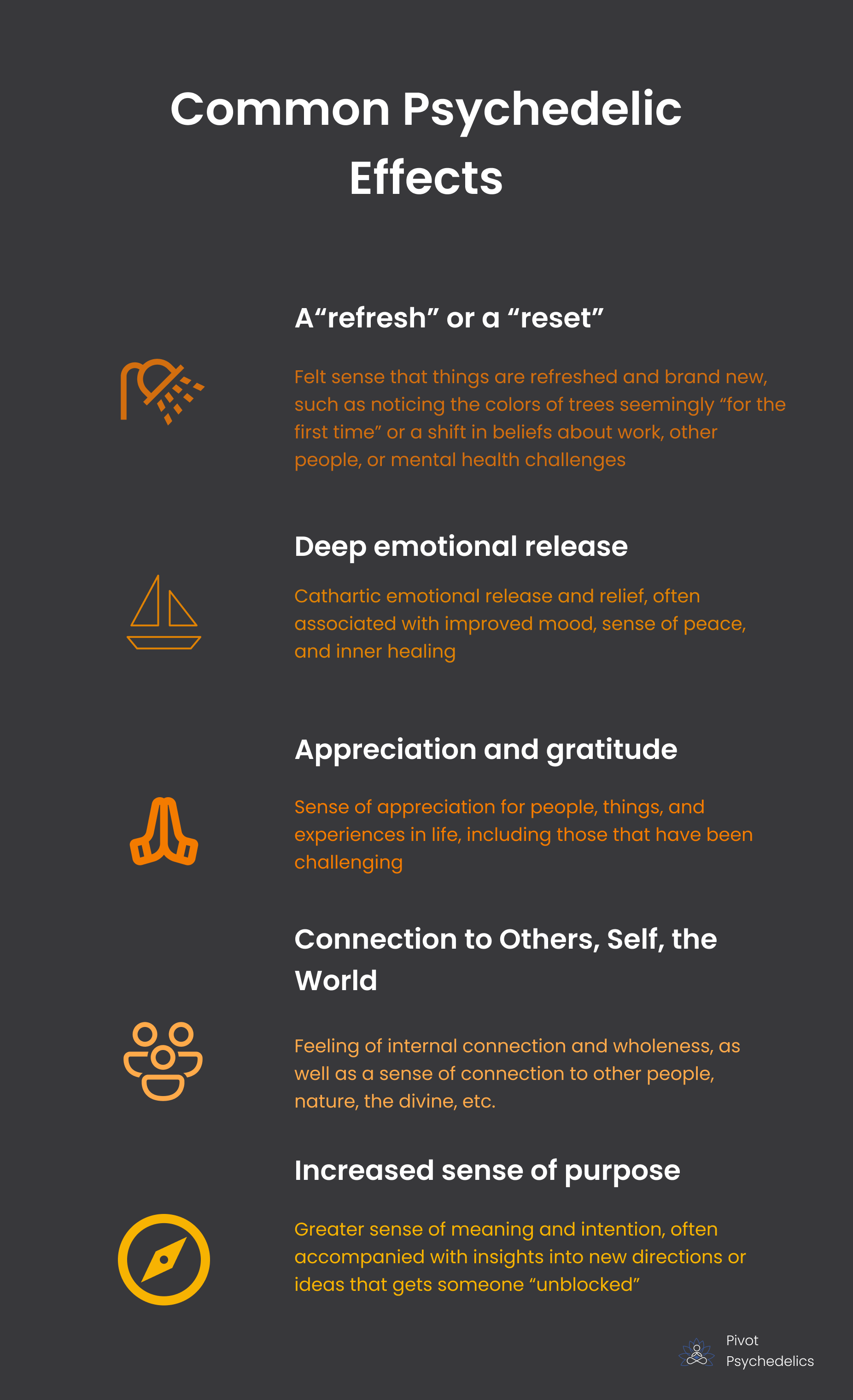
But how does it actually feel? What is it actually like to go through a psychedelic experience and work through depression?
Here are some of the most common findings we see working with clients who have depression after a psychedelic experience:
We know that psychedelics increase neuroplasticity, which allows the brain to form new neural connections. [15]
It seems that this effect leads to a return to basic, yet profound joys in life. People who engage with psychedelics can live with a more present-mind, rather than being burdened by anxiety, fear, worry, or sadness.
Research shows that intentional psychedelic use is associated with higher well being including:
Higher trait optimism
Positive affect
Self-esteem
Resilience
Psychological flexibility
Mindfulness
Many of these factors are inter-connected to improved mental health outcomes.
With sustained therapeutic support, these positive improvements can be even greater and last longer.
Your psychedelic guide will work with you to maximize these therapeutic benefits and create a container for healing.
Traditional vs. Clinical Use of Psychedelics for Depression
When we look at a psychedelic and its effect on the human brain, body, psyche, etc., we can consider it from a variety of perspectives.
From a traditional lineage perspective, some groups have used plant medicines for hundreds of years. And they've done so to treat ailments of the body, as well as the mind, spirit, and soul. For other groups, psychedelics are a rite of passage that mark an important moment in one's development.
Another perspective is the Western, clinical, medical one. This is what typically gets covered in the press and media. Most often when a research institution like UCLA or Johns Hopkins comes out with a study on psychedelic medicine and mental health, it falls under this clinical approach.
Since that's the framework from which most of our readers source information, we'll look at the voices and evidence from that perspective. We acknowledge that this view, while helpful for many, can also have limitations. At the same time, we know these substances are not without risks, and we advise anyone considering the use of psychedelic drugs to consult with a medical professional and act within the bounds of the law.
In our next section, we'll look at efficacy rates for addressing depressive symptoms and include discussion around spirituality and mysticism as it's studied alongside these metrics.
Best Psychedelics for Depression
When it comes to psychedelic drugs having a positive impact on depression, many of them have potential.
As mentioned, psilocybin treatment (e.g., combining psychedelic therapy with magic mushrooms) has demonstrated efficacy in clinical trials. For the last 20 years, psilocybin has been the focus of most psychedelic research in America.
Prior to this, scientists primarily studied LSD for clinical use. Several psychedelic books (CITE ARTICLE) from therapists, clinicians, and healers discuss this powerful molecule's efficacy.
Another synthetic "psychedelic" is 3,4-methylenedioxymethamphetamine abbreviated "MDMA" and known by its common names "ecstasy" or "molly". Technically it has a different effect from the classic psychedelics, such as psilocybin, LSD, and DMT, but it's felt effect is similar.
The Multidisciplinary Association for Psychedelic Studies (MAPS) is investigating the efficacy of MDMA-assisted therapy for the treatment of patients with severe PTSD.
They've completed Phase 3 Program Studies and seen great efficacy for the treatment of PTSD, which is often associated with depression, alcohol use, substance use, and/or childhood trauma. [16]
Ketamine is another molecule often lumped in with other psychedelic drugs. While it's not technically a psychedelic, it has similar effects and is approved for off-label use to treat depression and anxiety, making it extremely accessible for patients today.
Researchers have found ketamine effective for treating depression compared to other forms of treatment. [17]
One set of researchers at Stanford found that ketamine and a placebo worked equally well at reducing depressive symptoms in surgery patients who have severe depression. [18]
For many of these medicines, structured support coupled with intentional use outside of the research settings has strong anecdotal indicators of efficacy.
Ultimately, choosing to work with one psychedelic or another should be done in consultation with a physician to ensure safety and promote therapeutic benefits. Additionally, one should consider the legal status of these substances.
Why A Psychedelic Therapist or Guide Matters
A psychedelic experience can be beautiful. It can include mystical visions, happy memories, and a flood of positivity.
Usually though, the psychedelic experience isn't all "sunshine and rainbows". Most people report moments of challenge or trial during their experience.
What does this look like?
A variety of things can happen during a psychedelic experience and some people find these things difficult: lost sense of time, lowered ego, shaking or crying, and feeling like you are another person, spirit, or entity.
Now, for many individuals, these experiences are incredibly therapeutic, but they can be unnerving when they onset.
What separates a "challenging" experience form a "therapeutic" one are typically two factors:
Preparation, including setting expectations and practicing grounding techniques
Facilitation support, real time care and guidance from a therapist or sitter
For these two reasons, most people work with a guide or a therapist who knows the psychedelic landscape well.
This can be especially helpful for folks who are looking to address depression.
When it comes to preparation, the guide will help you explore your thoughts and beliefs around psychedelics and healing and provide insights into their accuracy.
Additionally, they will help you practice grounding techniques which can help in the psychedelic experience, as well as the rest of life. These could be practices like deep breathing, meditation, or repeating a mantra.
Your guide will support you during the actual psychedelic journey by providing deep compassion and wisdom as it's helpful. This high level of care and attention alone can be therapeutic, and in the context of a psychedelic experience it can help turn a challenging moment into an opportunity for healing.
Psychedelic healing doesn't stop after the ceremony. In some ways, it's just begun. For this reason we work with clients through the Psychedelic Integration Therapy Process to harness these powerful experiences and make the most out of them.
Disclaimer: While the body of research around psychedelic treatment for depression is growing, many substances remain federally illegal in the United States. None of the information presented in this article is an endorsement of illicit drug use. No content, including this blog past, from Pivot Psychedelics is medical advice nor an adequate substitute for it. Please consult with a medical professional if you are experiencing depression.
Sources:
von Rotz, R., Schindowski, E. M., Jungwirth, J., Schuldt, A., Rieser, N. M., Zahoranszky, K., Seifritz, E., Nowak, A., Nowak, P., Jäncke, L., Preller, K. H., & Vollenweider, F. X. (2022). Single-dose psilocybin-assisted therapy in major depressive disorder: A placebo-controlled, double-blind, randomised clinical trial. EClinicalMedicine, 56, 101809. doi:10.1016/j.eclinm.2022.101809
Depression. (2023, January 13th) Cleveland Clinic. www.my.clevelandclinic.org/health/diseases/9290-depression.
Voineskos, D., Daskalakis, Z. J., & Blumberger, D. M. (2020). Management of Treatment-Resistant Depression: Challenges and Strategies. Neuropsychiatric disease and treatment, 16, 221–234. doi:10.2147/NDT.S198774
Tupper, K. W., Wood, E., Yensen, R., & Johnson, M. W. (2015). Psychedelic medicine: a re-emerging therapeutic paradigm. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne, 187(14), 1054–1059. doi:10.1503/cmaj.141124
Baum, D. (2016, April). Legalize It All: How to win the war on drugs. Harper’s Magazine. www.harpers.org/archive/2016/04/legalize-it-all.
Cavarra M, Falzone A, Ramaekers JG, Kuypers KPC and Mento C (2022) Psychedelic-Assisted Psychotherapy—A Systematic Review of Associated Psychological Interventions. Front. Psychol. 13:887255. doi: 10.3389/fpsyg.2022.887255
Goodwin, G. M., Aaronson, S. T., Alvarez, O., Arden, P. C., Baker, A., Bennett, J. C., ... & Malievskaia, E. (2022). Single-dose psilocybin for a treatment-resistant episode of major depression. New England Journal of Medicine, 387(18), 1637-1648.
Zeifman, R. J., Wagner, A. C., Watts, R., Kettner, H., Mertens, L. J., & Carhart-Harris, R. L. (2020). Post-Psychedelic Reductions in Experiential Avoidance Are Associated With Decreases in Depression Severity and Suicidal Ideation. Frontiers in psychiatry, 11, 782. doi:0.3389/fpsyt.2020.00782
Mans, K., Kettner, H., Erritzoe, D., Haijen, E. C. H. M., Kaelen, M., & Carhart-Harris, R. L. (2021). Sustained, Multifaceted Improvements in Mental Well-Being Following Psychedelic Experiences in a Prospective Opportunity Sample. Frontiers in psychiatry, 12, 647909. doi:10.3389/fpsyt.2021.647909
Barber, G. S., & Aaronson, S. T. (2022). The Emerging Field of Psychedelic Psychotherapy. Current psychiatry reports, 24(10), 583–590. doi:10.1007/s11920-022-01363-y
Mayo Clinic Staff. (2019, September 17). Selective serotonin reuptake inhibitors (SSRIs). Mayo Clinic. www.mayoclinic.org/diseases-conditions/depression/in-depth/ssris/art-20044825.
Kennedy, S. H., Evans, K. R., Krüger, S., Mayberg, H. S., Meyer, J. H., McCann, S., Arifuzzman, A. I., Houle, S., & Vaccarino, F. J. (2001). Changes in regional brain glucose metabolism measured with positron emission tomography after paroxetine treatment of major depression. The American journal of psychiatry, 158(6), 899–905. doi:10.1176/appi.ajp.158.6.899
Goldapple, K., Segal, Z., Garson, C., Lau, M., Bieling, P., Kennedy, S., & Mayberg, H. (2004). Modulation of cortical-limbic pathways in major depression: treatment-specific effects of cognitive behavior therapy. Archives of general psychiatry, 61(1), 34–41. doi:10.1001/archpsyc.61.1.34
Psilocybin Treatment for Major Depression Effective for Up to a Year for Most Patients, Study Shows. (2022, February 15). Johns Hopkins Medicine. www.hopkinsmedicine.org/news/newsroom/news-releases/2022/02/psilocybin-treatment-for-major-depression-effective-for-up-to-a-year-for-most-patients-study-shows.
Calder, A.E., Hasler, G. Towards an understanding of psychedelic-induced neuroplasticity. Neuropsychopharmacol. 48, 104–112 (2023). doi:10.1038/s41386-022-01389-z
Mitchell, J.M., Bogenschutz, M., Lilienstein, A. et al. MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study. Nat Med 27, 1025–1033 (2021). doi:10.1038/s41591-021-01336-3
Anand, A., Mathew, S. J., Sanacora, G., Murrough, J. W., Goes, F. S., Altinay, M., Aloysi, A. S., Asghar-Ali, A. A., Barnett, B. S., Chang, L. C., Collins, K. A., Costi, S., Iqbal, S., Jha, M. K., Krishnan, K., Malone, D. A., Nikayin, S., Nissen, S. E., Ostroff, R. B., Reti, I. M., … Hu, B. (2023). Ketamine versus ECT for Nonpsychotic Treatment-Resistant Major Depression. The New England journal of medicine, 388(25), 2315–2325. doi.org/10.1056/NEJMoa2302399
Bai, N. (2023, October 19). Ketamine’s effect on depression may hinge on hope. Stanford Medicine News. www.med.stanford.edu/news/all-news/2023/10/ketamine.html.